December 06, 2024
A higher body mass index (BMI) in midlife is a significant risk factor for dementia. But a blanket measurement of body fat, like BMI, may not be the best predictor of cognitive decline, after all.
A new study, led by researchers at Washington University in St. Louis, suggests the link between body fat and brain health is more nuanced.
Their results are not yet published, but they suggest that deep belly fat is linked to markers of Alzheimer's years before cognitive symptoms begin to show.
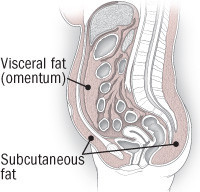
A more ubiquitous type of fat, called subcutaneous fat, could not explain the link between BMI and markers of dementia.
The findings were recently presented at the annual meeting of the Radiological Society of North America.
Lead author Mahsa Dolatshahi says the "crucial result" is that higher ratios of deep, visceral fat in a person's 40s or 50s is associated with amyloid protein clumps in the brain.
And while these plaques are not always a sign of Alzheimer's disease, they can be an early marker of cognitive decline.
"This study goes beyond using BMI to characterize body fat more accurately with MRI and, in so doing, reveals key insights about why obesity can increase risk for Alzheimer's disease," says Dolatshahi.
"Even though there have been other studies linking BMI with brain atrophy or even a higher dementia risk, no prior study has linked a specific type of fat to the actual Alzheimer's disease protein in cognitively normal people," Dolatshahi explained ahead of the conference.
Gathering studies suggest that some types of fat may be healthier than others, but many studies that investigate the link between obesity and dementia lump all types of fat together, or they only consider subcutaneous fat deposits, which are easier to measure and account for the vast majority of all fat in the body.
Visceral fat is inherently different. Not only is it stored deeper in the body, wrapping around organs, it can influence the production of cholesterol and insulin, and is linked to metabolic issues. To measure visceral fat requires magnetic resonance imaging (MRI).
In August, Dolatshahi and colleagues published their initial results from a pilot study of 32 adults in their 40s to 60s with normal cognition. Individuals with more visceral fat in their abdomen showed higher amyloid pathology in the right cortex of their brain, as well as a thinner cortex in some brain areas associated with Alzheimer's.
The trial was then extended. Researchers say their newest findings, which include data from 80 individuals, show that the ratio of visceral fat to subcutaneous fat in the belly is linked to increased amyloid in the brain, and that this accounts for 77 percent of the effect of high BMI on amyloid accumulation.
"To our knowledge, our study is the only one to demonstrate these findings at midlife where our participants are decades out from developing the earliest symptoms of the dementia that results from Alzheimer's disease," said Dolatshahi in November.
Interestingly, the team found lower levels of high-density lipoprotein (HDL) cholesterol – sometimes called 'good' cholesterol – were associated with greater amyloid levels in the brains of their participants.
Cholesterol production is influenced by visceral fat, and previous studies have linked cholesterol levels to dementia. In fact, earlier this year, researchers found too much of the 'good' cholesterol can increase the risk for dementia by as much as 42 percent in older adults.
A higher ratio of visceral fat was also associated with reduced insulin levels. Recently, a study found those with insulin resistance are susceptible to faster brain shrinkage, and that this double whammy substantially increases the risk of developing cognitive issues later in life.
Clearly, the link between the health of the body and the brain is extremely complicated, and far more research is needed before we can figure out why Alzheimer's develops more often in those with higher BMIs.
In the meantime, regular exercise and a healthy diet are two of the best ways a person can protect their brains and bodies from decline.
The findings were presented at the Radiology Society of North America's 2024 conference.